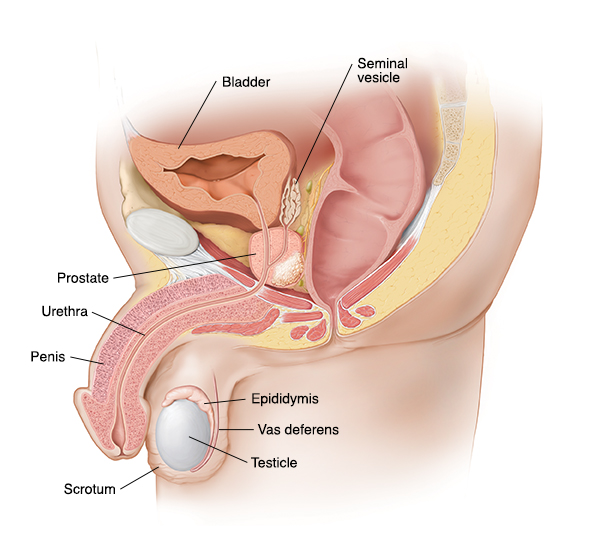
The male reproductive anatomy includes the penis, testes, vas deferens, and seminal vesicles. These organs produce, store, and transport sperm.
The male reproductive system plays a crucial role in human reproduction. It consists of both external and internal organs that work together to produce and deliver sperm. The penis and scrotum are the primary external structures. Internally, the testes produce sperm and testosterone.
The epididymis stores sperm until ejaculation. The vas deferens transports sperm from the epididymis to the urethra. Seminal vesicles, the prostate gland, and the bulbourethral glands produce fluids that mix with sperm to form semen. Understanding male reproductive anatomy is essential for reproductive health and family planning. Proper function and health of these organs are vital for fertility.
External Structures
The male reproductive system is a complex network of organs and structures. It plays a crucial role in human reproduction. The external structures of the male reproductive system are visible parts. They have important functions in sexual intercourse and protecting internal organs. Understanding these structures helps in knowing how the male body works.
Penis Anatomy
The penis is a vital part of the male reproductive system. It is the organ used for sexual intercourse and urination. The penis has three main parts:
- Root: The base of the penis, attached to the pelvic bones.
- Shaft: The long, cylindrical part of the penis.
- Glans: The rounded tip, often called the head.
The shaft contains three columns of erectile tissue:
- Corpora cavernosa: Two columns on the top side.
- Corpus spongiosum: One column on the underside, surrounding the urethra.
During arousal, these tissues fill with blood. This causes the penis to become erect. The glans is covered by the foreskin in uncircumcised males. The foreskin can be pulled back to expose the glans. The glans has many nerve endings, making it very sensitive.
Scrotum Role
The scrotum is a pouch of skin that hangs below the penis. It holds and protects the testicles. The scrotum has important functions:
- Temperature regulation: Keeps testicles cool for sperm production.
- Protection: Cushions the testicles from injury.
The scrotum is divided into two compartments. Each compartment holds one testicle. The scrotal skin has a muscle layer called the dartos muscle. This muscle contracts and relaxes to move the testicles closer or further from the body. When it is cold, the scrotum tightens to keep the testicles warm. When it is warm, the scrotum relaxes to cool the testicles down.
The scrotum also contains the spermatic cord. This cord includes blood vessels, nerves, and the vas deferens. The vas deferens is a tube that carries sperm from the testicles to the urethra. The scrotum’s ability to adjust temperature is key for healthy sperm production.
Credit: www.saintlukeskc.org
Internal Organs
The male reproductive system has several important internal organs. These organs work together to produce, store, and transport sperm. Understanding these organs helps us appreciate the complexity and efficiency of the male reproductive system. Let’s dive into the key internal organs and their functions.
Testes Function
The testes, or testicles, are two oval-shaped organs located in the scrotum. They have two main functions: producing sperm and making testosterone.
Sperm production happens in tiny tubes called seminiferous tubules. These tubes are coiled tightly inside each testis. Each testis has about 700 feet of these tubes! Sperm cells grow and mature as they move through these tubules.
Testosterone is the main male hormone. It’s crucial for developing male characteristics like a deep voice, facial hair, and muscle mass. The testes release testosterone directly into the bloodstream.
Here’s a table summarizing the key functions of the testes:
| Function | Description |
|---|---|
| Sperm Production | Happens in seminiferous tubules. |
| Testosterone Production | Essential for male characteristics. |
Both functions are vital for male fertility and overall health. Without the testes, the male body cannot produce sperm or enough testosterone.
Epididymis Structure
The epididymis is a long, coiled tube that sits on the back of each testis. It plays a key role in sperm maturation and storage.
Here’s a simple structure of the epididymis:
- Head: The top part, where sperm first enters.
- Body: The middle part, where sperm continues to mature.
- Tail: The bottom part, where mature sperm is stored until ejaculation.
The epididymis is about 20 feet long if stretched out! Sperm takes about three weeks to travel through it. During this time, they gain the ability to swim and fertilize an egg.
In the epididymis, sperm also get nutrients. This helps them survive and stay healthy. The tail of the epididymis connects to the vas deferens, which transports sperm during ejaculation.
Without the epididymis, sperm would not mature properly. This would make fertilization difficult or impossible. The epididymis ensures that sperm are ready for their journey.
Sperm Pathway
The male reproductive anatomy is a marvel of biological engineering. One of its most fascinating aspects is the sperm pathway. This intricate journey ensures the delivery of sperm from the testes to the outside world. Each step in this pathway plays a crucial role in reproduction. Understanding these steps can provide insights into male fertility and reproductive health.
Vas Deferens Journey
The vas deferens is a long, muscular tube that transports sperm from the epididymis. It begins at the tail of the epididymis and ascends into the pelvic cavity. The vas deferens is crucial for sperm motility and survival.
Here are some key points about the vas deferens journey:
- The vas deferens is approximately 30 cm long.
- It passes through the inguinal canal.
- It joins with the duct of the seminal vesicle to form the ejaculatory duct.
The journey of the sperm through the vas deferens involves several stages:
- Collection: Sperm is collected from the epididymis.
- Transportation: Smooth muscles in the vas deferens propel sperm forward.
- Transition: The vas deferens merges with the seminal vesicle duct.
The vas deferens also plays a role in storing and protecting sperm. Its muscular walls contract during ejaculation, ensuring efficient sperm delivery. This journey is vital for successful fertilization.
Seminal Vesicles Contribution
The seminal vesicles are two small glands located behind the bladder. They play a significant role in semen production. Each seminal vesicle contributes a fluid that mixes with sperm.
Key functions of seminal vesicles include:
- Producing a viscous fluid rich in fructose.
- Secreting prostaglandins which help sperm move.
- Adding alkaline fluid to neutralize the acidic environment of the vagina.
The seminal vesicle fluid has several components:
| Component | Function |
|---|---|
| Fructose | Provides energy for sperm |
| Prostaglandins | Stimulate uterine contractions |
| Alkaline fluid | Neutralizes vaginal acidity |
The seminal vesicles’ contribution ensures sperm viability and motility. Their secretions mix with sperm in the ejaculatory ducts. This mixture forms semen, which is then expelled during ejaculation. The seminal vesicles are essential for reproductive success.

Credit: lomalindafertility.com
Accessory Glands
The male reproductive system is a complex network of organs and glands. Among these, the accessory glands play a crucial role in reproductive health and function. These glands include the prostate gland and the bulbourethral glands, which produce vital fluids for sperm health and motility.
Prostate Gland Function
The prostate gland is a walnut-sized organ located below the bladder. It surrounds the urethra, the tube that carries urine and semen out of the body. The prostate gland’s main function is to produce a fluid that makes up part of the semen. This fluid helps nourish and transport sperm during ejaculation.
Here are some key functions of the prostate gland:
- Fluid Production: The prostate produces a milky fluid that is a part of semen.
- Enzyme Release: It releases enzymes that help liquefy semen after ejaculation.
- Antibacterial Properties: The fluid contains substances that help prevent urinary tract infections.
The prostate fluid is slightly alkaline, which helps neutralize the acidity of the vaginal tract. This environment is crucial for sperm survival. The table below summarizes the components of prostate fluid:
| Component | Function |
|---|---|
| Enzymes | Break down proteins in semen |
| Zinc | Antibacterial properties |
| Citrate | Nourishes sperm |
Bulbourethral Glands
The bulbourethral glands, also known as Cowper’s glands, are small pea-sized glands located near the base of the penis. They are situated below the prostate gland and are responsible for producing a clear, slippery fluid that is released before ejaculation.
Here are the primary functions of the bulbourethral glands:
- Lubrication: The fluid lubricates the urethra for sperm to pass through easily.
- Neutralization: It helps neutralize any acidic urine residue in the urethra.
- Pre-Ejaculate: The fluid, also known as pre-ejaculate, may contain sperm.
The fluid from the bulbourethral glands plays a significant role in sexual health. It prepares the urethra for the passage of semen, reducing friction and protecting sperm. This fluid also helps maintain a healthy pH balance in the urethra, creating a favorable environment for sperm.
Below is a summary of the key aspects of the bulbourethral glands:
| Aspect | Description |
|---|---|
| Size | Pea-sized |
| Location | Base of the penis |
| Function | Lubrication and neutralization |
Hormonal Regulation
The male reproductive system relies heavily on hormonal regulation. Hormones control many functions, from sperm production to sexual drive. Understanding these hormones helps us appreciate how the male body works. The main players in this process are testosterone, Follicle-Stimulating Hormone (FSH), and Luteinizing Hormone (LH).
Testosterone Production
Testosterone is the primary male sex hormone. It plays a crucial role in developing male reproductive tissues. This hormone is produced in the testes, specifically in the Leydig cells.
Testosterone affects various bodily functions:
- Development of male reproductive organs
- Growth of body hair
- Increase in muscle mass
- Deepening of the voice
- Libido and sexual function
The production of testosterone is regulated by the brain. The hypothalamus and the pituitary gland play key roles. The hypothalamus releases Gonadotropin-Releasing Hormone (GnRH). This hormone signals the pituitary gland to release LH and FSH.
Here’s a simple table showing the key elements:
| Element | Function |
|---|---|
| Hypothalamus | Releases GnRH |
| GnRH | Stimulates pituitary gland |
| Pituitary Gland | Releases LH and FSH |
| Leydig Cells | Produce testosterone |
Role Of FSH And LH
Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH) are essential for male reproductive health. They are produced by the pituitary gland and have specific roles in the reproductive system.
FSH is vital for sperm production. It stimulates the Sertoli cells in the testes. These cells support and nourish developing sperm cells. Without FSH, sperm production would be impaired.
LH stimulates the Leydig cells to produce testosterone. The increased testosterone levels, in turn, help in the maturation of sperm. LH ensures that testosterone levels remain adequate for proper reproductive function.
Below is a summary of their roles:
- FSH: Stimulates Sertoli cells
- LH: Stimulates Leydig cells
The interaction of FSH and LH ensures efficient sperm production and overall reproductive health. Maintaining a balance of these hormones is essential for fertility and normal sexual function.
Common Disorders
The male reproductive system is complex and vital for human reproduction. It includes structures such as the testes, prostate gland, and penis. Understanding common disorders affecting this system is crucial for maintaining men’s health. Two of the most prevalent issues are an enlarged prostate and testicular cancer.
Enlarged Prostate
An enlarged prostate, or benign prostatic hyperplasia (BPH), is a common issue in older men. The prostate gland surrounds the urethra and can grow larger with age. This growth can cause various urinary problems.
- Frequent urination, especially at night
- Difficulty starting urination
- Weak or interrupted urine stream
- Feeling of incomplete bladder emptying
Doctors use several methods to diagnose BPH. These include:
- Digital rectal examination (DRE)
- Urine tests
- Blood tests
- Prostate-specific antigen (PSA) test
- Ultrasound
Treatment options vary based on severity. Mild cases may need only lifestyle changes or medications. Severe cases might require surgical interventions.
| Medication | Purpose |
|---|---|
| Alpha-blockers | Relax prostate muscles |
| 5-alpha reductase inhibitors | Shrink the prostate |
Regular check-ups are essential. Early detection helps manage symptoms effectively.
Male Reproductive Anatomy
Testicular Cancer
Testicular cancer occurs in the testicles, which produce sperm and testosterone. It is most common in younger men, typically between ages 15 and 35. Early detection is key to successful treatment.
- A lump or swelling in the testicle
- Heaviness in the scrotum
- A dull ache in the lower abdomen or groin
- Sudden fluid collection in the scrotum
- Pain or discomfort in the testicle or scrotum
Doctors diagnose testicular cancer through physical exams, ultrasound, and blood tests for tumor markers. Treatment depends on the cancer stage and type.
- Surgery to remove the affected testicle (orchiectomy)
- Radiation therapy
- Chemotherapy
Regular self-examinations help detect changes early. Awareness and prompt action can save lives.
Aging Changes
The male reproductive system undergoes various changes as men age. These changes can impact both physical and mental health. Understanding these aging changes is crucial for maintaining well-being and quality of life. This section delves into the specific aspects of aging in the male reproductive system, focusing on decreased testosterone and erectile dysfunction.
Decreased Testosterone
Testosterone levels naturally decline with age. This hormone plays a vital role in many bodily functions. As men age, they may notice several changes due to decreased testosterone:
- Reduced muscle mass
- Increased body fat
- Lower energy levels
- Decreased libido
Symptoms of low testosterone can vary but may include:
| Symptom | Description |
|---|---|
| Fatigue | Feeling tired more easily |
| Mood changes | Increased irritability or depression |
| Sleep disturbances | Difficulty falling or staying asleep |
Managing decreased testosterone involves a healthy lifestyle. Regular exercise, balanced diet, and stress management can help. In some cases, doctors may recommend hormone replacement therapy (HRT).
Erectile Dysfunction
Erectile dysfunction (ED) becomes more common as men age. ED is the inability to achieve or maintain an erection. It can affect self-esteem and relationships. Causes of ED in older men can include:
- Poor blood flow
- Hormonal changes
- Medications
- Psychological factors
Symptoms of ED may include:
- Difficulty getting an erection
- Trouble maintaining an erection
- Reduced interest in sex
Treatments for ED are available and can include:
- Lifestyle changes like losing weight
- Medications such as Viagra or Cialis
- Therapy or counseling
Talking to a healthcare provider is important for proper diagnosis and treatment. Early intervention can improve quality of life.

Credit: www.healthdirect.gov.au
Reproductive Health
The male reproductive system is a complex network of organs and structures. It plays a crucial role in human reproduction. Understanding reproductive health is essential for maintaining overall well-being. Good reproductive health helps prevent diseases and ensures the proper functioning of the reproductive system.
Importance Of Check-ups
Regular check-ups are vital for maintaining male reproductive health. These visits help detect potential issues early. Early detection can prevent serious conditions and improve treatment outcomes.
Here are some reasons why regular check-ups are important:
- Early Detection: Identifies problems like infections or cancers early.
- Preventive Care: Helps in preventing diseases through vaccinations and lifestyle advice.
- Monitoring Health: Keeps track of overall health and any changes in reproductive organs.
Doctors may recommend specific tests during check-ups:
| Test Name | Purpose |
|---|---|
| Testicular Exam | Checks for lumps, swellings, or abnormalities. |
| Prostate Exam | Assesses prostate health and screens for prostate cancer. |
| STD Screening | Detects sexually transmitted diseases. |
Regular check-ups are essential for staying healthy. They provide peace of mind and ensure any issues are addressed promptly.
Healthy Lifestyle Choices
Making healthy lifestyle choices significantly impacts reproductive health. A balanced diet, regular exercise, and avoiding harmful habits contribute to overall well-being.
Consider these healthy lifestyle choices:
- Balanced Diet: Eat a variety of foods rich in vitamins and minerals.
- Regular Exercise: Engage in physical activities to boost circulation and reduce stress.
- Avoid Smoking: Smoking affects sperm quality and overall reproductive health.
- Limit Alcohol: Excessive alcohol can harm reproductive organs.
- Stay Hydrated: Drink plenty of water to maintain body functions.
Here are some foods that promote reproductive health:
| Food | Benefits |
|---|---|
| Leafy Greens | Rich in folate and antioxidants. |
| Nuts and Seeds | Provide essential fatty acids and vitamins. |
| Fruits | High in vitamins, especially vitamin C. |
Adopting healthy habits can enhance reproductive health. Focus on making small, consistent changes for long-term benefits.
Frequently Asked Questions
What Are The 7 Structures Of The Male Reproductive System?
The 7 structures of the male reproductive system are the testes, epididymis, vas deferens, seminal vesicles, prostate gland, bulbourethral glands, and penis.
What Is The Male Reproductive System Anatomy?
The male reproductive system includes the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and penis. These organs produce, store, and transport sperm. The system also produces male hormones like testosterone.
What Are The Main Parts Of Male Reproductive Anatomy?
The main parts include the testes, epididymis, vas deferens, seminal vesicles, prostate gland, and penis. Each part plays a specific role in reproduction.
What Is The Function Of The Testes?
The testes produce sperm and testosterone. They are essential for male fertility and secondary sexual characteristics.
Conclusion
Understanding male reproductive anatomy is crucial for overall health. This knowledge empowers better health decisions and fosters awareness. By learning about each part, we enhance our understanding of the body’s functions. Stay informed and proactive about reproductive health for a healthier life.
 Reproductive Health Sexual and Reproductive Health
Reproductive Health Sexual and Reproductive Health